Depression is the leading mental health cause of the global burden of disease, affecting 4.7% of the world’s population—approximately 450 million people. Yet the ability to treat this widespread condition is starkly unequal. While psychological treatments are recommended as first-line interventions by the WHO’s Mental Health Gap Action Programme, the reality on the ground tells a different story.
In low- and middle-income countries (LMICs), the treatment gap exceeds 90%. In India specifically, 85% of people with depression never receive treatment. The mathematics is brutal: India has approximately 0.3 psychiatrists per 100,000 population, compared to the WHO-recommended minimum of 3 per 100,000. Even in high-income settings, the treatment gap often exceeds 50%.
The barriers are both structural and economic. Supply-side constraints—severe shortage of mental health professionals—combine with demand-side challenges including low mental health literacy, stigma, and the prohibitive cost of specialist care. For decades, this gap was accepted as an unfortunate reality of resource constraints.
The annual global cost attributable to depression is estimated at $1.15 trillion, primarily through lost productivity and disability. For businesses and health systems, this represents not just a humanitarian crisis but an economic catastrophe that demands innovative solutions.
The Innovation: Task-Shifting to Lay Counselors
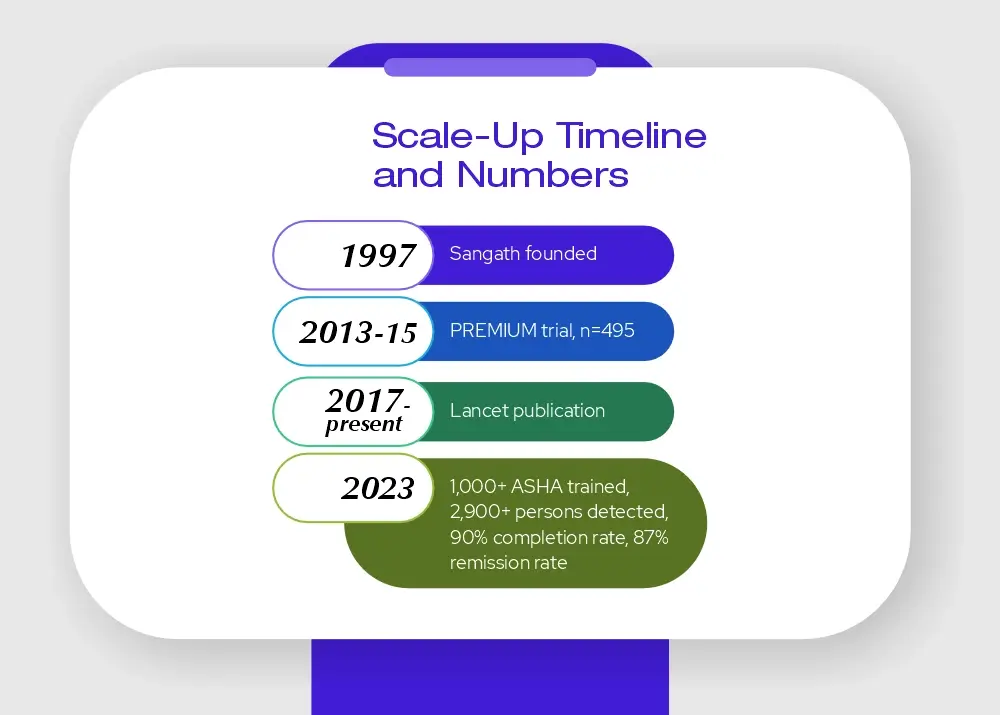
Enter Dr. Vikram Patel and Sangath, an NGO founded in Goa, India, in 1997. Patel’s radical proposition was elegantly simple: if there aren’t enough psychiatrists, train the people who are available. This approach, known as “task-shifting,” involves transferring specific tasks from highly specialized health workers to those with less training but appropriate supervision.
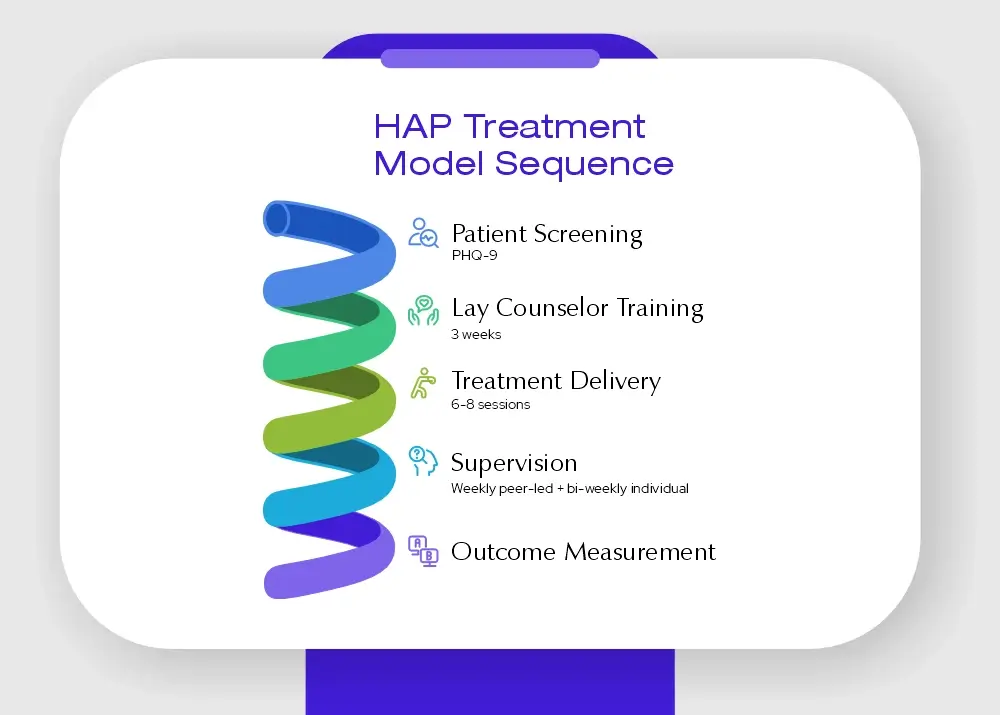
Through the Program for Effective Mental Health Interventions in Under-Resourced Health Systems (PREMIUM), Sangath developed the Healthy Activity Program (HAP)—a brief psychological treatment adapted from behavioural activation specifically designed for delivery by lay counselors in primary care settings.
What is Behavioural Activation?
Behavioural activation is an empirically supported psychological treatment recommended by WHO. Unlike complex cognitive therapies that require extensive training, behavioural activation focuses on helping patients engage in meaningful activities that improve mood and functioning. The HAP adaptation includes:
- Psychoeducation about depression
- Behavioural assessment and activity monitoring
- Activity structuring and scheduling
- Activation of social networks
- Problem-solving strategies
- Strategies to improve interpersonal communication
- Advice on sleep and tobacco cessation
Critically, HAP was condensed from the typical 20-24 session format into just 6-8 sessions of 30-40 minutes each, making it feasible for resource-constrained settings.
The Implementation: From Research to Reality
The Landmark Trial
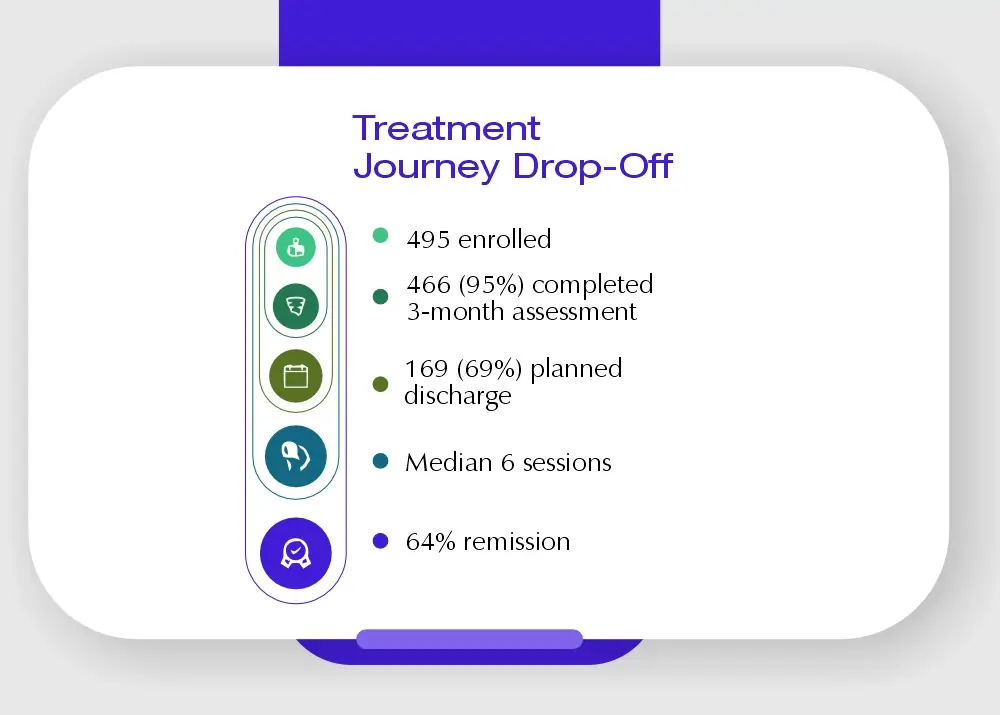
Between October 2013 and July 2015, Sangath conducted a rigorous randomized controlled trial across ten primary health centres in Goa. The study, published in The Lancet in December 2016, enrolled 495 participants with moderately severe to severe depression (PHQ-9 scores >14).
Participants were randomly assigned to either:
- Enhanced Usual Care (EUC) alone—standard primary care plus screening results and WHO mhGAP guidelines
- EUC plus HAP delivered by trained lay counselors
Who Were the Lay Counselors?
The intervention was delivered by 11 lay counselors who had no prior mental health training. These individuals received:
- A 3-week participatory workshop covering both HAP and counseling for alcohol problems
- A 6-month internship delivering treatments under supervision
- Weekly peer-led group supervision
- Twice-monthly individual supervision
- Ongoing quality assessment through recorded session reviews
This training model proved remarkably effective and scalable.
The Results: Evidence-Based Impact
The findings were striking across multiple dimensions:
Primary Clinical Outcomes
Depression Symptom Severity:
- HAP group: Mean Beck Depression Inventory-II score of 19.99
- Control group: 27.52
- Adjusted mean difference: -7.57 points (p<0.0001)
- Effect size: 0.48
Remission from Depression:
- HAP group: 64% achieved remission (PHQ-9 score <10)
- Control group: 39% achieved remission
- Adjusted prevalence ratio: 1.61 (61% increase)
- Number needed to treat: 4.15
This means that for every 4-5 patients treated with HAP, one additional person achieved remission compared to usual care.
Secondary Functional Outcomes
HAP showed superiority across all measured domains:
- Disability: Significantly reduced (effect size 0.13)
- Days Unable to Work: Reduced by 2.29 days per month (p=0.004)
- Behavioural Activation: Increased (effect size -0.39)
- Suicidal Thoughts/Attempts: Reduced by 39% (prevalence ratio 0.61)
- Intimate Partner Physical Violence (women): Reduced by 47% (prevalence ratio 0.53)
The reduction in intimate partner violence is particularly significant, as depression among women in India is strongly associated with gender disadvantage and domestic violence.
Treatment Completion and Quality
- 69% achieved planned discharge (completed treatment or met goals)
- Median sessions: 6 (IQR 5-7)
- 91% of follow-up sessions delivered at home (after initial PHC session)
- Mean session duration: 40.2 minutes
- Therapy quality scores: 2.58/3 (indicating good to average quality)
- 96% of sessions delivered face-to-face (vs. telephone)
Economic Analysis: The Business Case
From a health system perspective, the economic analysis revealed compelling value:
Cost per Patient (2015 International Dollars):
- HAP intervention cost: $66 per person
- Total health system cost (HAP + usual care): $113
- Total health system cost (usual care alone): $67
- Incremental cost: $46 per person
Cost-Effectiveness:
- Cost per Quality-Adjusted Life-Year (QALY) gained: $9,333
- Cost per remission: $181
- Cost per BDI point improvement: $6
According to WHO thresholds, interventions costing less than GDP per capita per QALY gained are considered highly cost-effective. HAP meets this standard with 87% probability of being cost-effective from a health system perspective.
The Societal Perspective
When considering broader societal impacts, the case becomes even more compelling:
- Productivity losses significantly reduced in HAP group vs. control
- From a societal perspective: HAP has a 98% chance of being cost-effective
- 42% chance of being cost-saving (lower costs AND better outcomes)
The reduced days unable to work translates directly to business productivity gains—a critical consideration for employers and economic planners.
Scaling Up: From Pilot to Policy
The success of the PREMIUM trial catalyzed systematic scale-up efforts across India:
IMPRESS: Implementation at Scale
Following the Lancet publication, Sangath launched IMPRESS (IMPlementation of evidence-based facility and community interventions to reduce the treatment gap for depRESSion)—the first systematic attempt in LMICs to scale up psychological treatment in primary care supported by evidence.
Real-World Implementation in Madhya Pradesh
As of 2023, the scale-up through India’s Accredited Social Health Activists (ASHA workers—India’s network of community health workers) has achieved:
- Over 1,000 ASHA workers trained in HAP delivery
- Close to 2,900 persons with depression detected and treated
- Approximately 90% treatment completion rate
- Over 87% remission rate at treatment end
These real-world outcomes mirror the controlled trial results, demonstrating the robustness and replicability of the intervention.
Government Integration
The program has successfully integrated with:
- India’s National Health Mission
- State-level primary health systems in Madhya Pradesh
- India’s first National Mental Health Policy (2014), which Dr. Patel helped draft
Key Success Factors: Why It Worked
1. Rigorous Evidence Base
The intervention was systematically developed using:
- Extensive formative research
- Cultural adaptation processes
- Pilot testing and refinement
- Gold-standard randomized controlled trial
- Publication in top-tier medical journals
2. Scalable Design
HAP was explicitly designed for scalability:
- Brief treatment protocol (6-8 sessions vs. 20-24)
- Deliverable by non-specialists with 3 weeks training
- Use of existing health workforce (ASHA workers)
- Integration into existing primary care infrastructure
- Peer-led supervision model reducing specialist burden
3. Cultural Appropriateness
Adaptations included:
- Home-based delivery options
- Pictorial patient resource materials
- Involvement of significant others/family members
- Strategies addressing local explanatory models of distress
- Focus on behavioural activation rather than complex cognitive work
4. Quality Assurance Systems
- Standardized training protocols
- Regular supervision (peer-led and specialist)
- Recorded session review and quality rating
- Continuous competency assessment
5. Economic Viability
The modest per-patient cost ($66 for intervention) is affordable even in resource-constrained settings, with strong ROI through reduced productivity losses.
Lessons for Global Mental Health
The Sangath HAP model offers transferable insights for health systems worldwide:
For Healthcare Systems:
- Task-shifting is not quality reduction—properly trained and supervised lay workers achieve outcomes comparable to specialist-delivered care
- Integration beats isolation—embedding mental health in primary care is more effective than parallel specialist systems
- Measurement matters—standardized screening and outcome measurement enable quality improvement
For Businesses and Employers:
- Productivity gains justify investment—reduced days unable to work and improved functioning translate to business value
- Prevention is economic—early intervention for depression prevents progression to disability
- Scalable solutions exist—evidence-based interventions can reach large employee populations
For Policy Makers:
- Evidence changes systems—rigorous trials published in prestigious journals catalyze policy adoption
- Local innovation travels—interventions developed in LMICs have relevance for high-income settings facing access challenges
- Community health workers are underutilized assets—with proper training, they can address mental health gaps
Challenges and Limitations
Despite remarkable success, challenges remain:
- Residual Depression: About one-third of participants remained depressed after treatment, suggesting need for stepped-care approaches
- Specialist Shortage Persists: While task-shifting helps, some patients still require specialist care
- Sustainability Questions: Long-term funding and system integration require ongoing commitment
- Measurement Discordance: Different depression scales showed somewhat different results, requiring careful interpretation
- Generalizability: While promising, replication in diverse settings with different health system structures is needed
The Road Ahead: Future Directions
Sangath and collaborators are pursuing several next-generation developments:
- Digital Enhancement: Online training platforms for HAP (available at nextgenu.org)
- M-Health Integration: Smartphone-based delivery and monitoring
- Reverse Engineering: Testing HAP effectiveness in high-income settings like the USA
- Broader Disorder Coverage: Extending task-shifting to other mental health conditions
- Long-term Follow-up: Assessing sustainability of outcomes beyond 3 months
Conclusion: A New Paradigm for Mental Healthcare
The Sangath HAP story represents more than a successful intervention—it demonstrates a paradigm shift in how we think about mental healthcare delivery. By challenging the assumption that quality mental health treatment requires highly trained specialists, Dr. Patel and his team have opened a pathway to closing the treatment gap that has plagued mental health for decades.
For business leaders, the message is clear: effective, scalable, affordable mental healthcare solutions exist. The depression treatment gap is not an unsolvable problem but a systems challenge with evidence-based solutions. The question is no longer “Can we afford to invest in mental health?” but rather “Can we afford not to?”
For health systems globally, the HAP model offers a blueprint: combine rigorous evidence, cultural adaptation, systematic training, quality supervision, and economic analysis to create interventions that work in the real world, not just in research settings.
Most importantly, for the millions living with untreated depression, the Sangath approach proves that where there is no psychiatrist, there can still be healing.